Trigger warning mentions of depression and suicide.

The semicolon has been one of the most prominent symbols of mental health and suicide prevention. A semicolon does not signify an end of a sentence but rather a connector of two independent clauses.
And just like in life, it indicates that mental health illnesses do not end either one’s story or life.
People from all walks of life have tattooed a semicolon on their bodies to bring awareness to the cause. It is also a way to show other people that they are alone in their plight.
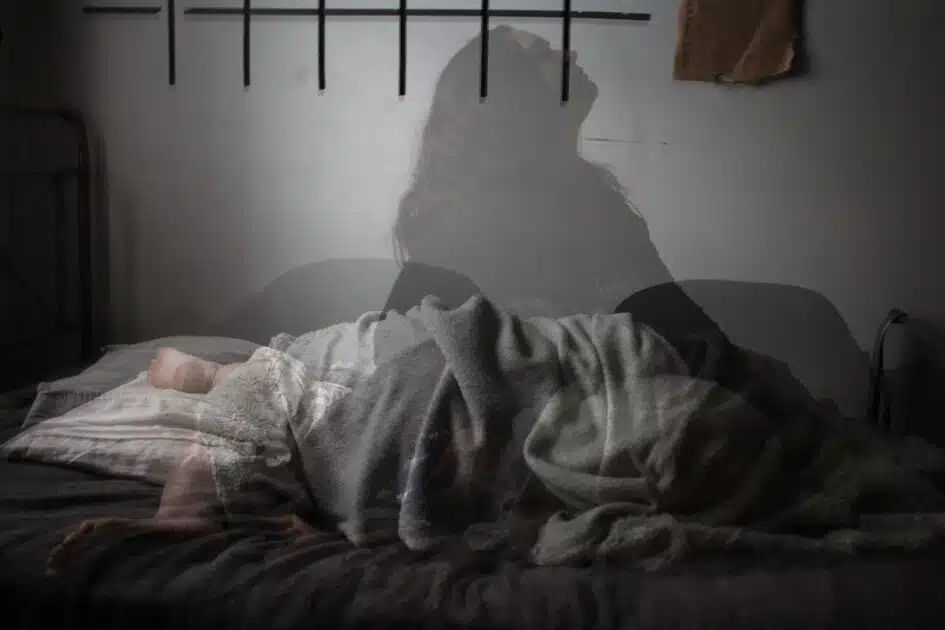
One famous phrase people use to describe how it feels to suffer from depression is the “black dog” metaphor. Having depression feels like having a big, intrusive, black dog who follows and tracks your every move and suffering.
The black dog follows you like a shadow, casting darkness on your entire life and rendering everything joyless and meaningless. As much as you want to break free from the dog, you can never run away from its darkness.
That is what having depression feels like – darkness that you can never escape.
What is depression?

There are many reasons why people complete suicide; however, depression plays a significant role in more than half of all suicide attempts. It is a prevalent mental disorder. 3.8% of the total population, almost 5% of adults worldwide, and 5.7% of adults older than 60 years old suffer from depression.
Additionally, it is already the leading cause of disability globally. It is a massive contributor to the overall global burden of disease.
According to the American Psychiatric Association, depression can arise at any point in a person’s life; however, on average, depression often initially appears during the late teens to mid-20s.
Women are also disproportionately affected by this as compared to men. Several studies conclude that one-third of women will experience major depressive episodes.
There is a lot of stigma around mental health illnesses, especially depression. Often, people post or say that people with depression are just extra sensitive, lazy, and attention-seekers. Sometimes, they even go as far as saying that they deserve to suffer.
However, depression is an actual medical condition – it is as severe and real as cancer and other deadly diseases. At the same time, nobody ever deserves to suffer from this paralysing mental illness.
We cannot and should not deny that depression is one of the leading mental health illnesses that have caused the spike in suicide cases worldwide.
In 2019, suicide was the 15th leading cause of death worldwide, with 759,028 casualties. This also means that half of 759,028 deaths are influenced by depression.
But what exactly is suicide? It has been used too many times in conversations and social media, and, in a way, it has lost its true essence. Depression is not just the feeling of sadness or pain; it is a severe medical illness that negatively affects how a person feels, thinks, and acts.
Yes, people experiencing constant sadness or emotional distress can have depression. However, some other criteria and symptoms must be present to diagnose depression as listed in the DSM-5.
What are the symptoms of depression?
You have heard of major depressive disorder (MDD) or seasonal depressive disorder (SAD). But did you know that there are seven types of depression? I’m sure you’re surprised, so let’s look into each class and its symptoms.
MAJOR DEPRESSIVE DISORDER (MDD)
When someone declares that they have “clinical depression,” they are most likely generally referring to MDD. It is a mood disorder that has several key symptoms:
- Depressed mood
- Lack of interest in activities that used to give them joy in the past
- A significant change in weight (losing or gaining)
- Changes in sleeping patterns
- Fatigue
- Feelings of worthlessness and guilt
- Difficulty concentrating
- Thoughts of death and suicide
A person who experiences most of these symptoms for longer than two weeks will often be diagnosed with MDD by a professional.
PERSISTENT DEPRESSIVE DISORDER (PDD)
PDD referred to as Dysthymia, is a chronic (i.e. long-term) depression that can last for years. Its symptoms may come and go over years, and their intensity (i.e. mild, moderate, severe) can also fluctuate.
What makes it persistent is that symptoms usually don’t disappear for more than two months at a time. Worse, people with PDD can also suffer from MDD, which is sometimes called double depression.
PDD can inflict significant impairment to the person, and its symptoms are:
- Loss of interest in daily activities
- Sadness, emptiness, or feeling down
- Hopelessness
- Tiredness and insufficiency of energy
- Struggle to concentrate and trouble making decisions
- Increased irritability or excessive anger
- Decreased activity, effectiveness, and productivity
- Avoidance of social activities
- Feelings of guilt and worries over the past
- Poor appetite or overeating
- Irregularities and challenges in sleeping
Bipolar disorder was previously called “manic depression” because of the mood episodes of bipolar range from extreme highs (mania or hypomania) and extreme lows (depression). There are four types of bipolar:
- Bipolar I disorder – A person should have at least one manic episode that may be preceded by a hypomanic or depressive episode. For some people, mania can trigger psychosis where they lose touch with reality.
- Bipolar II disorder – A person should have at least one major depressive episode and one hypomanic episode, but never a manic episode.
- Cyclothymic disorder – An adult, for at least two years, or a child or teenager, for at least one year, should have experienced multiple periods of hypomania and depressive symptoms. The depressive symptoms, however, should be less severe than major depression.
- Other types of bipolar and related disorders are induced by specific drugs or alcohol. At the same time, some are caused by medical conditions like stroke, multiple sclerosis, etc.
The depressive period under the bipolar is the same as in MDD. However, manic and hypomanic episodes include at least three or more of these symptoms:
- Abnormally upbeat, jumpy, or wired
- Increased activity, agitation, or energy
- Euphoria or an exaggerated sense of self
- Decreased need for sleep
- Unusual chattiness
- Racing thoughts
- Distractability
- Poor decision making
Bipolar is a lifelong condition; however, mood swings and other symptoms are always manageable if one follows a treatment plan.
Many mothers often feel guilty for not feeling empty for anything and anyone after delivering their baby. However, if sadness, hopelessness, or emptiness do not go away for longer than two weeks after giving birth, they may have postpartum depression.
PDD is a severe mental illness that impacts a person’s behaviour and physical health. People with PPD may feel disconnected from the baby or feel like they are not the actual mother or do not love and care for their baby.
In addition to this, many mothers also experience anxiety disorders during pregnancy.
Indeed, it is challenging to be a woman, especially a mom! Truth be told, one in nine mothers suffer from postpartum depression. Symptoms of PDD are:
- Feeling restless or moody
- Feeling sad, hopeless, or overwhelmed
- Constant crying
- Having thoughts of harming the baby
- Having thoughts of hurting yourself
- Not having any interest, connection, or positive feelings towards the baby as if it’s not yours.
- Having zero to little energy or motivation
- Eating too little or too much
- Sleeping too little or too much
- Challenge in focusing or making decisions
- Encountering memory problems
- Feeling worthless, guilty, or like a bad mother
- Losing interest in things/activities you used to enjoy
- Isolating from friends and/or families
- Experiencing headaches, aches, and pains, or stomach issues that won’t go away
Mothers rarely tell anyone about this, which makes the situation worse, but always keep in mind that these are not your thoughts but the illness’ thoughts. Always seek help and support from professionals and loved ones.
PREMENSTRUAL DYSPHORIC DISORDER (PMDD)
PMS is hard enough, so imagine suffering from PMDD every time of the month. PMDD adds extreme irritability, anxiety, or depression to the mix of your PMS symptoms, such as bloating, headaches, and breast tenderness. In fact, 10% of women are affected by PMDD globally.
Symptoms of PMDD appear a week or two before the start of your menstrual cycle and will go away a few days after it starts. In addition to PMS, a person may experience:
- Anger or irritability
- Anxiety and panic attacks
- Depression and suicidal thoughts
- Difficulty concentrating
- Fatigue and low energy
- Food cravings or binge eating
- Headaches
- Insomnia
- Mood swings
Healthcare providers will always look at one’s medical history and evaluate their symptoms. When they see five or more PMDD symptoms, including one mood-related sign, they will diagnose a person with PMDD.
This is very common and popular for people living in cold countries or places where the sun rarely appears, such as in northern areas. As the name suggests, SAD is a depression significantly related to seasonal changes.
It usually begins and ends at the same time every year. People with SAD typically experience symptoms from fall to winter and stop during the spring and summer months. While very rare, some experience SAD during spring and summer on the flip side.
The symptoms of SAD are the same as other types of depression, only with the variability of seasons and the inclusion of:
- Experiencing carbohydrate cravings, overeating, and weight gain for fall and winter SAD
- Poor appetite and weight loss for summer and spring SAD
Interestingly, people diagnosed with Bipolar Disorder have a higher risk of having SAD.
As the name suggests, the atypical disorder is a type of depression with atypical features. It is a subtype of MDD and PDD that includes several particular symptoms and is considered a “specifier” for these.
Atypicality includes increased appetite or weight gain, changes in the sleeping cycle, fatigue and lack of energy, moods that are forcibly reactive to environmental circumstances, and extreme rejection sensitivity.
The primary signifier of atypical depression is mood reactivity, which means that people with atypical depression experience improvement in their mood if something positive happens. Aside from this, other symptoms are:
- Sleeping too much or hypersomnia
- A significant change in eating habits
- An intense reaction or sensitivity to rejection often results in social and work-related problems.
- Having a feeling of being weighed down, paralyzed, or leaden
The diagnostic criteria require at least two of these symptoms to be classified as an atypical disorder.
How would you know if it’s just sadness or already clinical depression?

Sadness is a normal human emotion that everyone experience throughout their lives. Sadness is a natural reaction to situations that cause pain, disappointment, or hopelessness.
Of course, there are also varying degrees of sadness. When you fail an exam, your sadness will undoubtedly be different from the sadness you’ll feel when a beloved pet dies. What’s important to note is that sadness is temporary and will naturally go away in time.
This is the main difference between sadness and depression: sadness fades away, but depression is a long-term mental illness. In addition, depression is also a disability that impairs a person’s social, occupational, and other areas of functioning.
Yes, there are times that sadness will last forever; however, extremely sad people can still smile, laugh, or be comforted at times.
While depression, like the black dog, affects all aspects of a person’s life, rendering them unable to find any glimpse of joy in life.
Is it safe to diagnose yourself with a mental health condition?

TikTok influencers have popularised and even normalised self-diagnosis. It is understandable for other people who come from a low economic background and do not have the means to access help.
There is a reason, however, why mental health professionals exist. Self-diagnosis poses more dangers than benefits. Self-diagnosis is the process of diagnosing or identifying a specific condition with yourself.
People would often go online and look for medical conditions and see if they have the symptoms. Unfortunately, people’s self-diagnosis is often wrong and can lead them astray.
Moreover, it can be perilous when a person self-diagnoses themselves and then jumps into a treatment plan independently. The treatment plan for the condition that they might not even have might harm their overall health.
The internet is often the source of information for people to diagnose themselves. It is a known fact that the internet is designed in terms of keywords and algorithms.
There is already a universal running joke that when you search for a symptom as simple as “headache” on the internet, the web will probably show you that you might have some form of cancer.1
So always do yourself a favour: when you feel like you are experiencing symptoms you read online, go to your trusted medical professional for proper diagnosis and treatment.
What are the primary causes of depression?

There are various reasons why people develop mental health illnesses, and people react to these very differently. Many people who experienced significant traumatic events have developed mental illness, but others did not.
Some people did not go through any critical traumatic event but still developed a mental health illness. Mental health illness is a combination of biological, social, and psychological factors, so it’s essential to go to mental health professionals for diagnosis and help.
There are plenty of elements that increase a person’s chances of developing clinical depression, such as:2
- Physical, sexual, or emotional abuse
- Age – Older people have a higher risk of depression, exacerbated by other factors such as living alone or lacking social support.
- Specific medication – Some drugs can increase the risk of depression.
- Conflict – Conflict can be personal or conflict with other people.
- Death or loss – Death or loss of a loved one, regardless of the cause, can increase the risk of depression.
- Gender – Women are more at depression risk. Hormonal changes are said to contribute to it in a way.
- Genes – A family history of depression may increase a person’s risk of developing depression.
- Significant events – Examples are losing a job or income, getting divorced, retiring, etc.
- Other personal problems – These may include social isolation, bullying, or being cast out by family members.
- Serious illness – Depression can also happen with other significant diseases or triggered by another medical condition.
- Substance misuse – Drugs and alcohol may make you feel better at use. However, it aggravates the feelings of depression right after. Almost 30% of people with substance misuse problems also have major or clinical depression.
How does depression affect members of the LGBT community?

It is not only women who are more at risk for developing depression; members of the LGBT community are also known for suffering from depression.
Living in a society filled with hatred, discrimination, and stigma towards LGBT members, many queer people experience abuse, conflict, traumatic events, social isolation, and bullying.
According to a report released by the Human Rights Campaign Foundation, LGBTQ youth are more likely to struggle with their mental health than non-LGBTQ youth. This is said to be caused by stigma and discrimination.
Here are the harrowing statistics on mental health and the LGBT community:
- Transgender youth are nearly four times more at risk than non-transgender peers of experiencing depression.
- LGBTQ teens remarkably experience depression more than their heterosexual peers.
- A 2016-2017 survey reported that 28% of LGBT youth and precisely 40% of transgender youth have stated that they have felt depressed almost all the time during the previous 30 days. This is a stark difference from non-LGBT youth, where 12% reported that they have felt depression during the last 30 days.
- Another 2015 survey on Youth Risk Behaviour Survey revealed that 60% of LGBT youth reported being incredibly hopeless or sad to the extent that they stop their usual activities.
- LGBT youth are twice as suicidal and four times more likely to attempt suicide than other heterosexual youth. Additionally, these suicidal rates are higher for bisexual teens.
- Of transgender youth, one-third have seriously considered suicide, while one in five has attempted suicide.
Queer people, especially the youth, are very vulnerable to depression and suicidal ideation. They need strong social support from their family, school, community, and other groups to cope.
In fact, LGBT youth from least accepting families are more likely to attempt suicide than those from accepting families.
The LGBT youth are not the only sector at risk of depression. LGBT adults are also more likely than others to suffer from mental health illnesses such as substance use problems or depression.
As a matter of fact, 13% of LGBT adults living with mental illness have a serious medical condition that notably interferes with their major life activities. Additionally, 40% of adult transgender adults have attempted suicide compared to less than 5% of the US population.
The most significant factor in the higher depression risk of LGBT members is stigma. A study done in 2014 found that LGBT people who live in communities with more stigmatised attitudes towards sexual orientation die an average of 12 years earlier than LGBT people who live in a more accepting society.
How can you help or support someone with depression?

Unfortunately, the topic of mental health is still taboo in most places. If not taboo, people are often not aware or educated enough on how to properly support people with depression.
People are scared that they might say the wrong things that will make matters worse or that they also do not have the emotional bandwidth to help the other person. All these reasons are valid.
But if you can help but just don’t know what to do, here are five simple things to keep in mind:
- Learn to see the signs of depression and always encourage treatment. It’s hard to help a loved one from depression if we are not aware they have depression. What makes it more complicated is that people who are going through depression also tend to isolate themselves from people or hide what they are truly going through.
So always stay vigilant to quickly spot if your loved one is going through something. You can offer emotional support by checking up on them or inviting them to hang out, but what they need is professional treatment.
You can subtly tell them that you notice that they are acting differently and are concerned about them. Then explain (if they are not aware) that it can be a medical condition requiring professional treatment.
Always express your willingness to help and that you will be there for them every step of the way. - Identify warning signs of worsening depression. If they are still not seeing a professional, this is the time to be provided more encouragement to see one.
- Understand suicide risks and learn suicidal first aid. It is a known fact that most people who have attempted or completed suicide have depression.
So know the signs of suicidal ideation and never be scared of taking action whenever you deem necessary. Open up to the person about your concern, or directly contact their family or health care provider when you feel that the situation asks for it. - Talk to them compassionately and listen actively. Sometimes, all a person needs is someone to talk to. Some people with depression just want to be seen, recognized, heard, and loved. Offer this to the person, and listen with open ears about their problems.
- Always prioritise your own mental health. Helping and supporting a loved one with depression isn’t an easy task. Always remind yourself that only they can save themselves, and all you can offer is support and help.
Prioritise your own mental health, and do not over-exert yourself. Continue to do things that give you joy, like eating your favourite food, traveling, continuing your hobby, or even talking to a therapist of your own!
At the end of the day, always be patient with the person with depression. It’s a complex, painful, and debilitating illness, and it’s hard to recover from it. They need all the support they need as they go through the darkest time of their lives.
And for people with depression, always remember that you can always put a leash and tame a dog. With proper therapy and enough social support, you will one day see a spark of light and learn techniques on how to tame the big, black dog. There is always hope.
HELP HOTLINES
If you are experiencing any suicidal ideations or any symptoms of mental illness, do not hesitate to seek help from a mental health professional.
If you are going through a crisis, you may call the following suicide hotlines:
USA – 1-800-273-8255 (available 24/7)
UK – 0800 689 5652 (available from 6 PM to 3:30 AM)
You may also access a comprehensive list of suicide crisis lines on this website.
Alternatively, you can also talk and seek support from your friends and follow the list of things to do when you are feeling suicidal.























